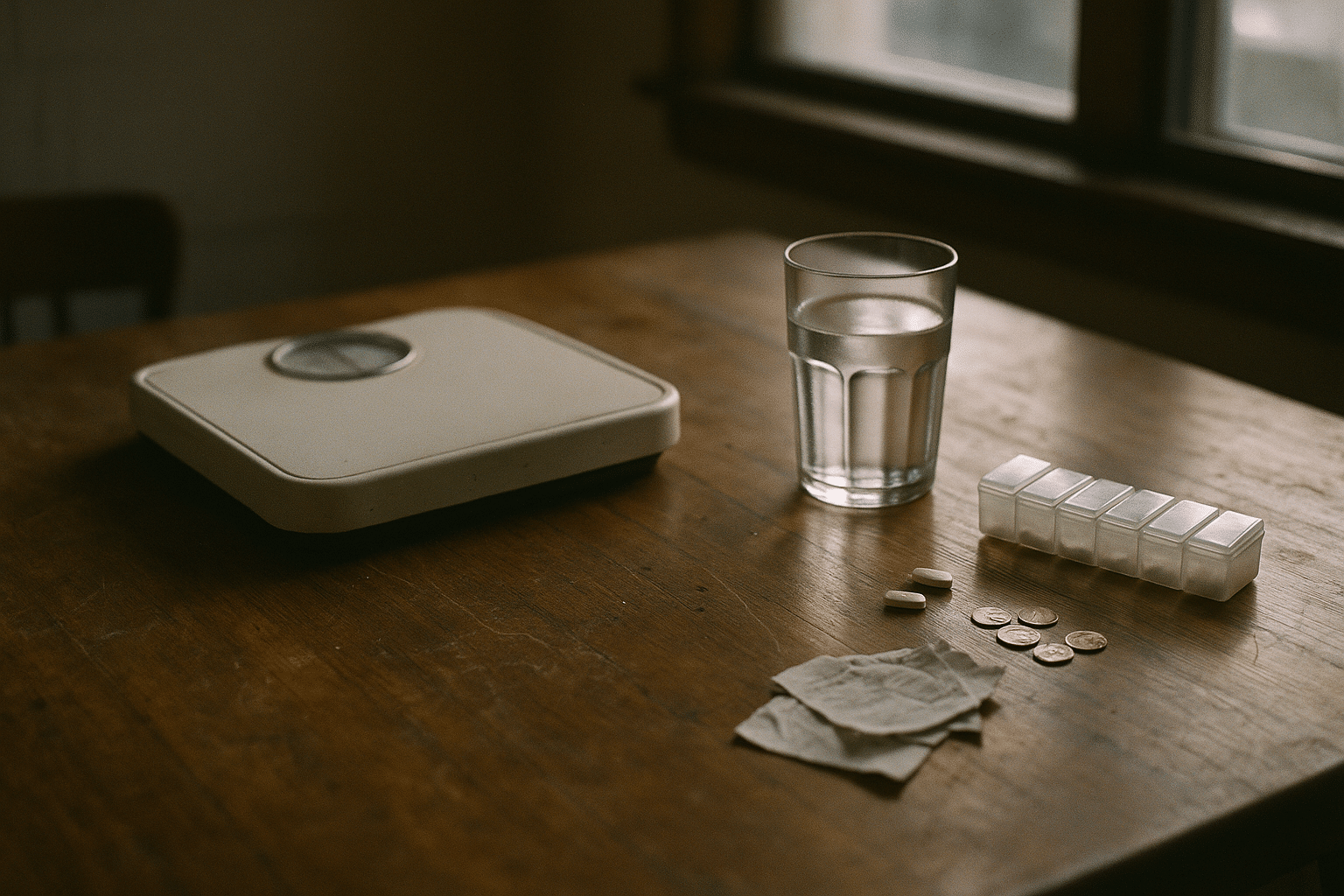
Weight Loss Pills What It Really Costs and Medication Available
Outline and Why Costs Matter Now
– Outline: What weight loss pills can and cannot do; medication classes and how they work; real efficacy and safety; true costs beyond the sticker price; step-by-step decision path to choose, budget, and use them responsibly.
– Why this matters: More people are considering medication to manage weight, yet the conversation often ends at “How much per month?” The real answer includes clinic visits, lab tests, titration periods, side-effect management, and how long you can safely and affordably stay on therapy. And because different drugs have different price tiers, mechanisms, and expected results, comparing them without context can be misleading. This section sets the stage by explaining how to frame the topic so you can read the rest of the guide with clarity.
Let’s start with a simple lens: total value over time. The direct price of a pill or injection is only one line among many. There are refill schedules, dose changes, supplies (for injectables), the cost of more fruits and vegetables if your appetite shifts, and time costs for ongoing follow-ups. Insurance rules can either smooth the road or turn it into a maze of prior authorizations, step therapy, and eligibility criteria based on body mass index and weight-related conditions. Without that bigger picture, it’s easy to chase a low copay and end up with a plan that stalls after the first refill, or choose a high-impact option that becomes unsustainable once introductory discounts end.
Practical takeaway for the journey ahead:
– Keep expectations anchored: medication supports weight loss; it does not replace nutrition, activity, sleep, and stress management.
– Budget at least a quarter ahead: many people experience dose changes in months two to four, which can alter costs and tolerability.
– Measure outcomes you care about: beyond the scale, track waist circumference, energy levels, blood pressure, and glucose markers if relevant.
– Plan an exit, even if you stay on therapy: understand how you would taper or transition if costs rise or side effects persist.
With this framework, the next sections walk through how each option works, what results to expect, and how to tally what it truly takes—financially and practically—to commit.
How Weight Loss Pills Work: Classes, Mechanisms, and Who They Suit
Weight loss medications aren’t a single thing; they’re a toolkit. Different classes target appetite, absorption, or metabolic signaling, and people respond differently based on health history and habits. Understanding mechanisms helps you set realistic expectations and match the option to your goals and constraints.
– Gastrointestinal lipase inhibitors (example: orlistat) block some fat absorption in the gut. Mechanism: less dietary fat enters your bloodstream. Expect modest weight loss support if you’re following a reduced-fat diet. Common trade-offs: oily stools, urgency, and fat-soluble vitamin loss, which may require supplementation.
– Sympathomimetic appetite suppressants (example: phentermine) reduce hunger via central nervous system stimulation. They can be helpful short term. Trade-offs: possible insomnia, elevated heart rate or blood pressure, and not appropriate with certain cardiovascular conditions or during pregnancy.
– Combination approaches include a sympathomimetic with an anticonvulsant (phentermine plus topiramate) or a dopamine/norepinephrine modulator with an opioid receptor antagonist (bupropion plus naltrexone). These aim to reduce appetite, cravings, and reward-driven eating. Common side effects vary by component: tingling, altered taste, mood changes, or nausea are reported.
– Glucagon-like peptide-1 (GLP-1) receptor agonists slow gastric emptying and signal satiety in the brain, typically resulting in reduced intake. Some agents are daily; others weekly. Nausea and fullness are common early on and often improve with gradual titration and mindful meal pacing. Cautions include a history of pancreatitis or certain thyroid conditions.
– Dual agonists (targeting both GIP and GLP-1 receptors) extend the signaling concept and have produced notable weight reductions in clinical trials. Like GLP-1 agents, gradual dose increases help manage gastrointestinal effects.
Who is a candidate? Generally, adults with a body mass index of 30 or higher, or 27 or higher with a weight-related condition such as elevated blood pressure, dyslipidemia, or impaired glucose regulation. A thoughtful clinician will also consider your medication list, mental health history, sleep patterns, and personal preferences. Some agents are not appropriate during pregnancy or for those with significant uncontrolled hypertension, seizure disorders, or certain endocrine conditions. While off-label options exist (for example, metformin in individuals with insulin resistance), a risk–benefit conversation is essential.
The big picture: mechanisms guide expectations. A gut-focused drug supports fat reduction from meals; a central suppressant reduces hunger and snacking; a hormone-mimicking agent reshapes satiety and portions. None of them delete the need for supportive habits. However, when aligned with lifestyle and monitored carefully, they can tilt the odds toward sustainable change.
Efficacy, Safety, and Comparisons You Can Actually Use
Results vary by class, dose, and adherence, but some patterns have emerged across trials and real-world use. Think in ranges and probabilities rather than guarantees.
– Gastrointestinal lipase inhibitors often yield a few percentage points of additional weight loss over lifestyle alone after a year, especially when dietary fat is moderated. Side effects are gastrointestinal and highly diet-dependent; keeping meals lower in fat lowers the chance of oily stools and urgency.
– Sympathomimetic agents can support meaningful short-term loss, particularly during the first three to six months, but long-term use depends on cardiovascular safety, blood pressure, and sleep quality. Common issues include restlessness and elevated heart rate; these require monitoring. Combining with behavioral strategies helps maintain momentum if a plateau arrives.
– The phentermine plus topiramate combination has shown larger average reductions than monotherapy in many studies, frequently in the high single to low double-digit percent range over a year, depending on dose and adherence. Side effects may include tingling, cognitive slowing, or altered taste; dose adjustment can mitigate these.
– The bupropion plus naltrexone combination often produces mid single to high single-digit average reductions, with some individuals doing better. Nausea and headache are common early side effects; taking doses with food and stepwise titration help many patients continue.
– GLP-1 receptor agonists often reach high single to low teens percentage reductions at full dose with consistent use and lifestyle support. Gastrointestinal symptoms are frequent early on; slowing eating pace, prioritizing lean proteins, and avoiding large, high-fat meals reduces discomfort for many people. There are rare but important cautions regarding pancreatitis history and certain thyroid tumors.
– Dual GIP/GLP-1 agonists have reported even higher average reductions in controlled settings—often in the mid to high teens and, in some cohorts, approaching about one-fifth of initial body weight. Real-world outcomes can be lower than trial results due to interruptions, cost, and dose constraints, but the class has demonstrated strong signals for both weight and cardio-metabolic markers.
Safety and monitoring: whatever you choose, plan structured follow-ups. Typical practice includes baseline measurements (weight, waist, blood pressure), labs if indicated (lipids, A1c or fasting glucose, liver and kidney function), and visits every 4–12 weeks during titration. High-yield strategies include:
– Use the slowest titration that still moves you forward.
– Track a few behaviors (protein intake, step count, meal timing) alongside the scale to catch plateaus early.
– Reassess at 12 and 24 weeks: if there’s less than about 5% loss by 12 weeks on a therapeutic dose, reconsider the plan.
– Anticipate the “what if I stop?” question. Regain is common if behaviors and supports drop; create a maintenance plan before you need it.
Plainly said: average ranges offer a map, not a promise. Your route depends on dose, consistency, side-effect tolerance, and the scaffolding of daily habits.
What It Really Costs: Sticker Price, Hidden Line Items, and Long-Term Math
Price tags grab attention, but a realistic budget includes more than the pharmacy counter. Here is a grounded, United States–focused range of typical monthly medication costs, noting that geography, insurance, dose, and supply affect totals:
– Gastrointestinal lipase inhibitor (generic): roughly $20–$100.
– Sympathomimetic (generic): roughly $10–$40.
– Combination components as separate generics (example, bupropion plus naltrexone; phentermine plus topiramate not in extended-release form): roughly $20–$80 total, depending on dose and pharmacy pricing. Extended-release combinations can be higher.
– GLP-1 receptor agonists: often $800–$1,400 without coverage.
– Dual GIP/GLP-1 agonists: commonly $900–$1,100 or more without coverage.
Hidden and variable costs matter just as much:
– Clinic visits: $100–$250 per visit for primary care or weight management follow-ups (frequency: every 1–3 months during titration).
– Lab work: $50–$200 per panel when paying cash; employer or community screening programs may reduce this.
– Supplies for injectables: alcohol swabs, sharps container, and travel storage; plan $5–$20 quarterly if not provided.
– Side-effect management: anti-nausea or constipation remedies, $5–$30 per month if needed.
– Nutrition shifts: higher-protein foods and produce can increase grocery bills by $20–$60 monthly for some households, though eating fewer restaurant meals may offset this.
Insurance and payment strategies can tilt the math:
– Many plans require a body mass index threshold and at least one weight-related condition for coverage, plus documentation of lifestyle efforts.
– Prior authorization and step therapy are common; budget extra time for approvals and potential interim prescriptions.
– Health savings or flexible spending accounts can cover eligible expenses; ask your plan which items qualify.
Scenario planning clarifies choices:
– “Lean-cost path”: generic sympathomimetic or lipase inhibitor, primary care follow-up, and community labs. Estimated monthly total: $50–$200 including visits averaged over a quarter.
– “Balanced path”: generic combination components with structured nutrition support. Estimated monthly total: $100–$250 plus periodic visits and labs.
– “High-impact path”: GLP-1 or dual agonist. Estimated monthly total: $900–$1,600 without coverage; $25–$200 with coverage, depending on copays and deductibles.
Zooming out, there is the opportunity-cost argument: sustained weight loss of 5–10% is associated with improvements in blood pressure, glucose control, and joint symptoms for many people. Some estimates suggest individuals with obesity spend over a thousand dollars more per year on healthcare than peers at lower weights, but savings are not immediate or guaranteed. Your decision is ultimately a value question: which path is financially sustainable and medically appropriate for you over the next 12–24 months?
Conclusion, Choices, and a Practical Action Plan
Choosing a weight loss pill is less about chasing a headline result and more about matching a realistic plan to your life. The smartest move is to stack small advantages—an agent with a mechanism that fits your eating pattern, a titration schedule your body tolerates, and a budget you can maintain through ordinary setbacks like travel or a busy season at work.
Use this decision flow to simplify the process:
– Clarify your main goal: appetite control, portion size, craving reduction, or meal-fat handling. Your goal hints at the right class.
– Screen for safety: pregnancy plans, cardiovascular status, seizure history, pancreatitis risk, and thyroid considerations can rule in or out entire classes.
– Check coverage before starting: ask your plan for criteria, approved doses, and whether you must try another agent first.
– Price the full quarter: medication, visits, labs, and supplies. If the three-month total strains your budget, consider a lower-cost class or a staged approach.
– Plan your habits: protein target, step count or activity minutes, a sleep window, and two high-impact meal routines you can repeat on autopilot.
– Set review points: at 12 weeks and 24 weeks, confirm progress. If weight loss is under 5% at a reasonable dose, revisit dose, adherence, or switch classes.
Cost-saving ideas that keep safety first:
– Ask about generics and whether non-extended-release components are acceptable.
– Consider 90-day fills if your insurer lowers the per-month cost and your dose is stable.
– Shop transparent-cash pharmacies; prices can vary widely.
– Use community lab pricing and combine tests with routine annual checks to avoid duplicates.
Finally, avoid shortcuts that risk your health: do not source medications from unknown sellers, do not mix agents without clinician oversight, and report new or severe symptoms promptly. Medications work best as part of a system that includes food quality, movement, stress skills, and sleep. When you align the right mechanism with your needs, budget for the real costs, and track the outcomes that matter to you, the numbers become clearer—and your plan becomes sturdier. That’s the kind of steady, sustainable progress that can genuinely change the way you feel day to day, not just the way the scale looks on a single morning.


